Research Program
The Raleigh Laboratory studies the genetic basis of developmental pathway misactivation in cancer. By focusing on cancer predisposition syndromes resulting from germline genomic alterations, our work aims to shed light on fundamental mechanisms of developmental biology and tumorigenesis. Most recently, we have interrogated molecular mechanisms underlying cancers associated with Gorlin syndrome or neurofibromatosis, cancer predisposion syndromes resulting from misativation of the Hedgehog pathway or inactivation of neurofibromatosis tumor suppressor genes, respectively. Our research makes use of biochemistry, molecular biology, cell biology, mouse genetics, genomics, bioinformatics, cerebral organoids, and pharmacology to gain new insights into the molecular determinants of human malignancies. To accomplish these multidisciplinary goals, the Raleigh Laboratory fosters broad collaborations with other laboratories and clinicians at UCSF and abroad. Some of our frequent collaborators include
The Abate Laboratory, UCSF Department of Bioengineering
The Costello Laboratory, UCSF Department of Neurological Surgery
The Hervey-Jumper Laboratory, UCSF Department of Neurologica Surgery
The Gilbert Laboratory, UCSF Department of Urology
The Krogan Laboratory, UCSF Department of Cellular and Molecular Pharmacology
The McCormick Laboratory, UCSF Department of Cellular and Molecular Pharmacology
The Reiter Laboratory, UCSF Department of Biochemistry & Biostatistics
The Rich Laboratory, UPMC Department of Medicine
The Schmitt Laboratory, MSKCC Department of Radiation Oncology
The Weiss Laboratory, UCSF Department of Neurology
The Xu Laboratory, University of Washington School of Pharmacy
Our research extends from broad investigations of tumor heterogeneity to basic studies of lipid signaling. With respect to the latter, our work has revealed novel activators and effectors of oncogenic Hedgehog signaling in medulloblastoma, the most common malignant brain tumor in children and a common cancer in patients with Gorlin syndrome. The Hedgehog pathway is transduced through primary cilia, and we used lipidomic mass spectrometry to identify cilia-associated seterol lipids that bind to Smoothened and activate oncogenic Hedgehog signaling. This discovery affords us the opportunity to study how lipids drive other Hedgehog-associated cancers, and may teach us how lipids regulate development. We found Hedgehog signaling induces CDK6 to drive medulloblastoma, lipid signaling mechanisms that mediate resistance to CDK6 inhibitors in medulloblastoma, and enzymes producing Smoothened-activating lipids that localize to the ciliary base. Ongoing work is focused on understanding the connections between ciliary Hedgehog signal transduction and Hedgehog target gene expression, and oncogenic lipids driving basal cell carcinoma, another Hedgehog-associated tumor that is the most common tumor in the United States.
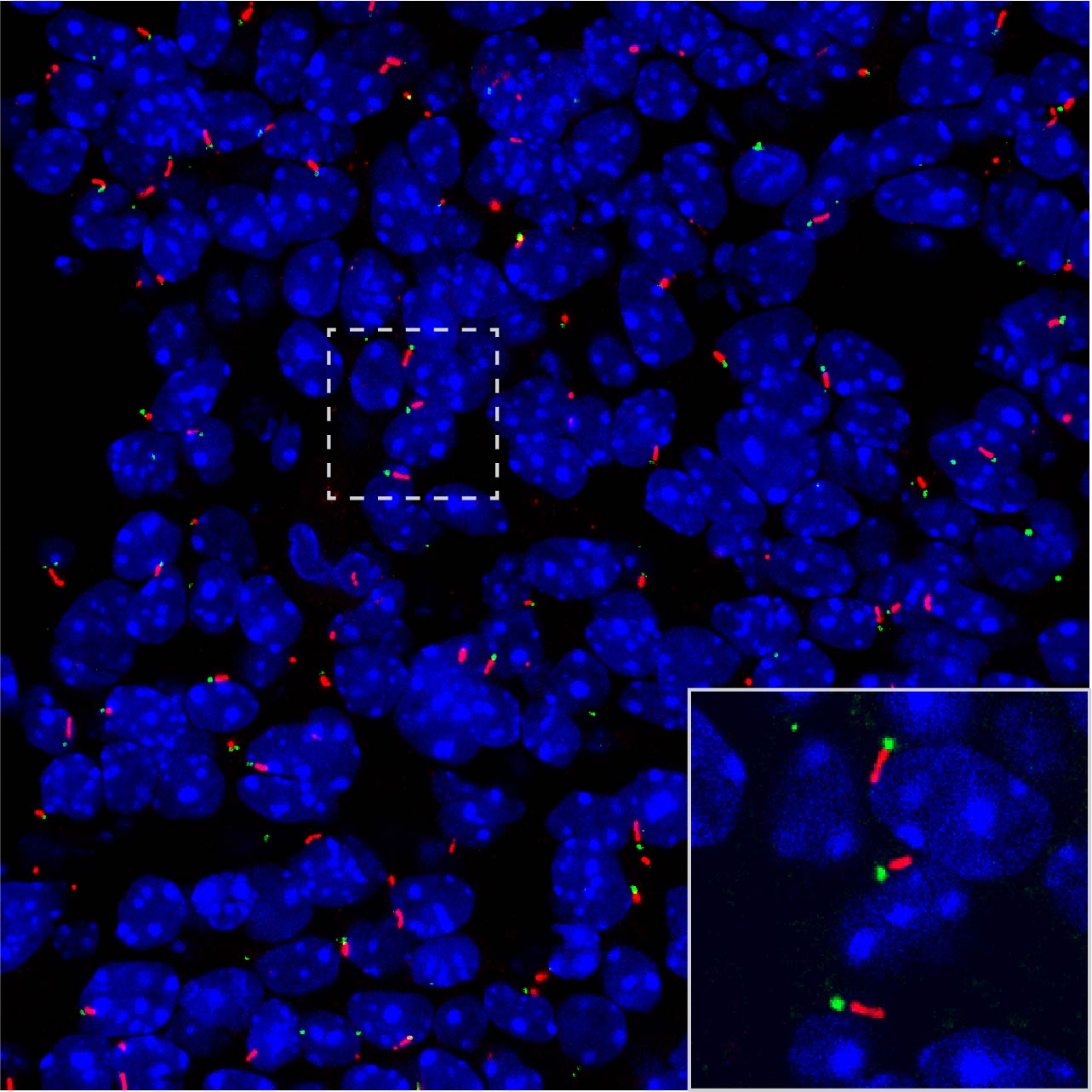
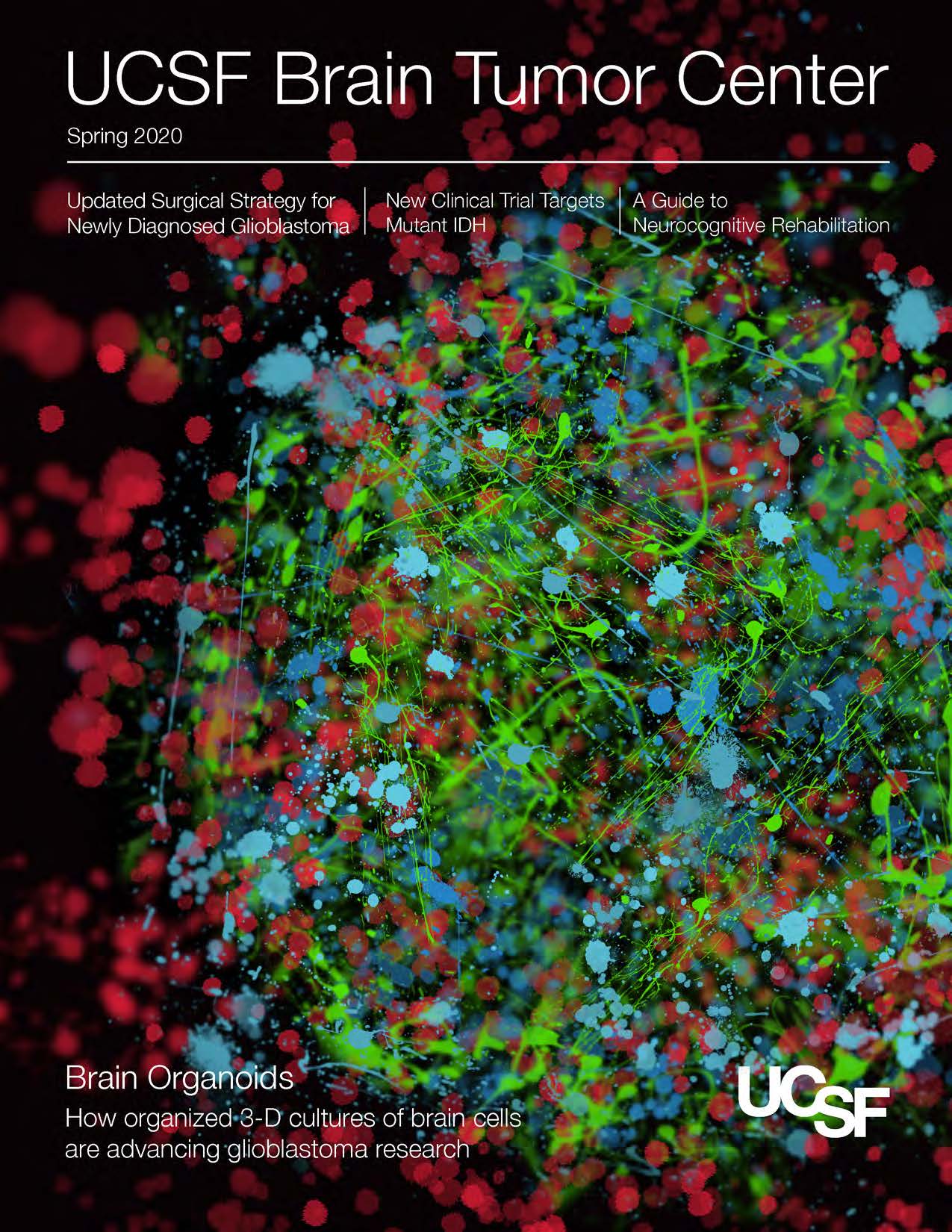
With respect to our investigations of tumor heterogeneity, we identified a FOXM1/Wnt signaling axis that drives cell proliferation in meningioma, the most common primary intracranial tumor in adults and a common cancer in patients with neurofibromatosis. Building on these foundational data, we are using single cell technology and cerebral organoids to study heterogeneity in meningioma and other cancers derived from the neural crest, a multipotent embryonic cell population that exhibits remarkable molecular diversity. In doing so, we have identified an epigenetic basis for intra-tumor heterogeneity in ependymoma; progenitor cell populations in glioblastoma that mimic cell types in the developing brain; molecular subgroups of meningiomas and malignant peripheral nerve sheath tumors; and epigenomic reprogramming mechanisms that underlie neural crest and immune subgroups of schwannoma.
Raleigh Lab Press
UCSF Press Release related to this video and this video!
NIH National Cancer Institute Cancer Currents Blog